The East of England Stroke Telemedicine Stakeholder Partnership has been delivering consultant expertise to the bedside of stroke patients for a decade. So, it has valuable experience to pass on to NHS stroke networks that want to do the same. Telemedicine manager Lynda Sibson and clinical lead Raj Shekhar pass on their top tips.
The East of England Stroke Telemedicine Stakeholder Partnership has been delivering a successful thrombolysis service to patients with acute ischaemic stroke for a decade.
It was set up in 2010 to meet national targets for getting clot-busting drugs to eligible stroke patients.
A shortage of stroke physicians made it impractical to offer a 24-hour consultant service at every hospital. So, a decision was made to use digital technology to support a rota of skilled consultants who could provide expert advice remotely.
Now, when a suspected AIS patient arrives out of hours at one of the seven hospitals supported by the partnership, a cart is taken to their bedside by a base team, which sets up a video link to the specialist stroke consultant on call, using Visionable’s technology.
Related case study: East of England celebrates ten years of better stroke care with Visionable.
The consultant has access to high-quality scans and can use the link to interact with the patient and the base-team. Ten years on, the service has assessed 4,311 patients. Of these, 1,852 were thrombolysed; and just a fifth of those who weren’t thrombolysed missed the national 4.5 hour target; while the rest saw their condition change or were not experiencing an AIS.
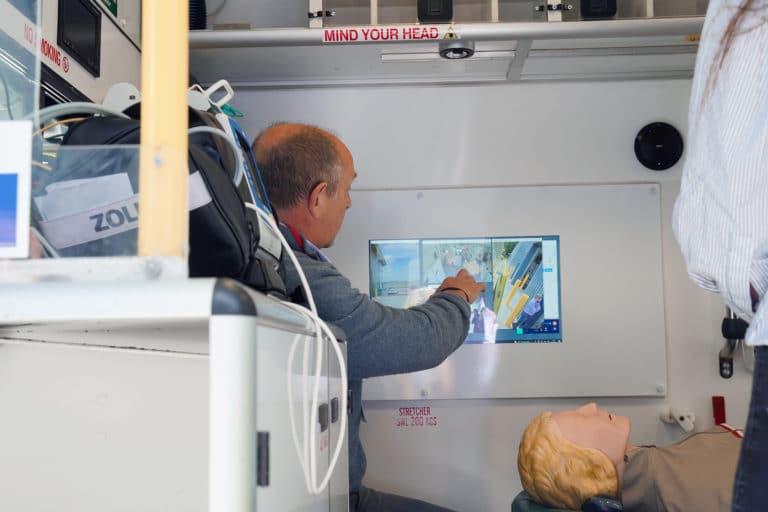
A health economic review by the University of East Anglia has shown that the service is cost-effective and delivers better outcomes for patients than usual care. And it is expanding. The partnership is working with ambulance crews to help them spot ‘stroke mimics’ that don’t require immediate transfer to A&E and with hospitals to review stroke patients on the ward, using mobile technology.
So, as stroke networks across the country look to improve their services, and NHS specialties of all kinds look to make more use of remoting working and virtual consultations following the Covid-19 pandemic, what should they learn from the East of England Stroke Telemedicine Partnership’s experience?
Lynda Sibson, the partnership’s telemedicine manager, and Raj Shekhar, its clinical lead and consultant at The Queen Elizabeth Hospital Kings Lynn, set out six lessons they have learned:
1. Clinical engagement is essential
Raj: “You need a network of consultants to agree that this is a good thing to do. It was difficult to get consultants to join at the start, so we really worked on governance and on generating feedback so we could prove we were benefiting patients. Now, for some of our newer consultants, this is the norm. Telemedicine is medicine.”
Lynda: “You also need clinical champions at each hospital. Our lead stroke nurses play that role. Getting nurses on board is critical, because there is no point doing a remote consultation if there is nobody on the ground to deliver the recommended care.”
2. Get the basics right
Lynda: “Co-ordination needs to be somebody’s job. Each hospital that uses our service has to provide at least one consultant, and somebody needs to make sure they are rotered so every shift is covered and everybody is supported. You need to get local IT involved, so they can provide support with networks and logins and laptops if necessary.
“You need to have one phone number, so the local clinical teams don’t have to remember numbers for individual consultants. You need to have a cascade of phones, so there are no issues with people not getting through. Because the base team has to be confident the service will be there if they are going to keep using it.”
3. Training matters
Raj: “Junior doctors are a challenge. They need to recognise the symptoms of stroke and when to refer, and it can be hard to make sure they can do that when they are undertaking shorter and shorter rotations as part of their training. So, we are really working on that and developing educational resources for them.
“But you need training for everybody in the base team. The radiology team that loads the scans into the system. The specialist nurses who will be at the bedside. You have to set standards for the competency you expect, because each consultation is only 15-17 minutes long. So, you don’t want anybody saying ‘oh, I’ve never done this before’ during a consultation, because time is so important.”
4. You need the right technology
Raj: “The technology has to be in place before you launch a service like this. It’s not just the cart, and the video streaming, and the scans. You need good wi-fi, you need laptops with high resolution screens. You need good IT support.”
Lynda: “Visionable is really good at providing software that is easy to use at 3am. When time is against you, the system has to be easy to use. And being able to see the patient really matters.
“Using Visionable’s technology, the stroke consultant on call can see the patient and talk to their family and base team. They can talk through the assessment and see care being delivered. A lot of hospitals that say they run a telemedicine service give their doctors a data feed or access to scans remotely. That is not telemedicine.”
5. Consultations must be captured in the patient record
Raj: “Another important aspect of this service is that we can use the software to create a record of the consultation. To comply with information governance guidelines, we have to make sure that we do not capture, store or transmit any identifiable patient information during the teleconsultation.
“But information is captured in an anonymised audit form and can be printed for the patient record. It’s not like a telephone call where you provide support but there is no case note.
“Those reports also create data, which is great, because it can be audited and reviewed to improve care. Our service is based at Addenbrookes Hospital in Cambridge, which doesn’t use the service, because it has 24/7 consultant cover, but it still wants to be involved because it feels it is benefiting from the data that we generate.”
6. Success creates success
Raj: “A service like this is complex and it won’t run smoothly in the first week or two. It takes six months or so to bed-in. However, over time, we have been able to see the impact of what we have achieved.
“We can see the numbers building up and think: ‘wow’. And we can see the treatment getting better and better. Analysis shows that we have no ‘weekend effect’ and no day/night effect. Our patients get the same treatment at the weekend as they do during the week and at night as they do during the day.
“However, the best thing is to see a patient who has used this service walking down the corridor a few days later. That is a great thing, professionally. Knowing that rapid treatment got them a great outcome, and that on two thirds of any day that service is being delivered by telemedicine.”
Statistics accurate as of March 2021.