Despite digital adoption becoming more widespread in healthcare, the quality of stroke care is regressing. Technology is increasingly having a positive impact to boost service levels, lighten the load on a strained workforce and improve patient outcomes. However, recent reports suggest that stroke care is slipping backwards as the NHS faces the challenge of post-COVID recovery. This is even more reason to look at applying technology to the pathway rapidly but in a smart way.
Our recent roundtable brought together health leaders from across the NHS to discuss the role that technology plays within nursing and therapist communities in stroke care. It was a lively and wide-ranging discussion, with many interesting takeaways.
Here, I have summarised the priorities and questions discussed at the roundtable to consider how we can further leverage technology to improve the stroke pathway.
1. Are resources being allocated effectively to improve stroke care?
Health leaders are asking: how can we ensure resources are being put to where we can get the most benefit? There is a clear discrepancy between where resources should be vs. where they are going. Tackling this challenge involves empowering providers and giving them a more direct ability to influence where resources go. Provision is often driven by bio medical models, but we should be using real-time data to make resource-based decisions.
We can use the digital era and its generation of data to help us align resources to need. This is a major breakthrough but will require a culture change, not just in the NHS but also in the public accepting this.
-
Managing the workforce shortage challenge
A prominent example of misalignment in resource allocation is the workforce shortage. The healthcare industry is rapidly losing workers in key areas whilst not using capacity in others.
Technology adoption is the most important way that we can maintain services and meet demand with the resources available. We must use technology for productivity and to help us transform pathways, avoid stroke in the first place and diagnose it accurately at first presentation. This requires staff to be trained and to adopt a positive mindset towards the use of technology but very often they are so busy that they have little time to adopt ways of being less busy and more productive. This needs leaders to engage and inspire staff to see technology and change as the answers to their demand problems not a distraction from them.
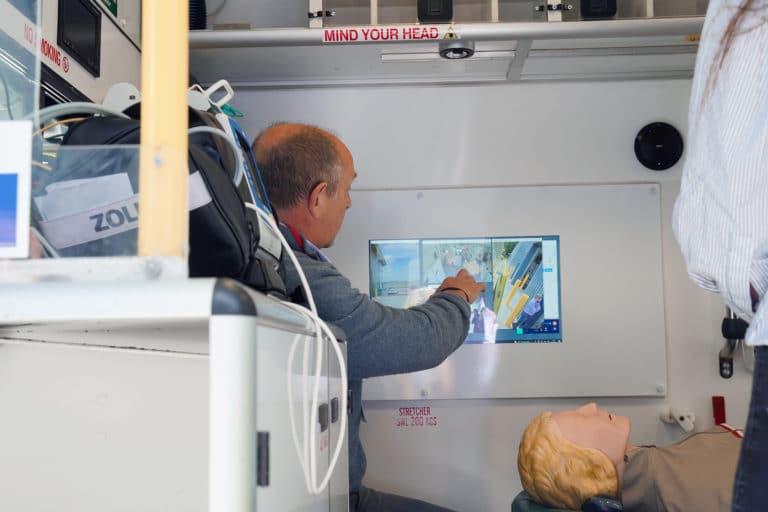
Similarly, digital solutions such as virtual and tele-rehab are increasingly utilised and highly valued. Therapists in the hospital can extend their reach geographically and extend the amount of time they can take with patients, which is a major step forward to deliver rehabilitation to more people.
-
Stroke care operational constraints
There are significant operational constraints with moving patients through the pathway in line with what would be deemed fit with their medical condition to avoid readmission. Crucially, there are gaps in the system that mean there is a lack of support in vital areas, mostly in post-acute stage, such as clinical psychologists and rehab nurses. As such, there can be instances where patients ‘can’ go home rather than ‘should’ go home.
We discussed the need to use the facilities that we have for the patients that really need them, however, this is not always easy to determine when looking at things in siloes. Technology can help by providing a bird’s eye view of the entire system through real-time dashboard data and intelligence, empowering clinicians to make decisions and ensuring patients do not stay in hospital longer than needed.
-
Resource allocation with patient outcomes at the core
Patients need to feel the benefit of resource management, for example, improved provision of certain treatments and continuity of care. Patients benefit if they have a named rehabilitation nurse to stay with them throughout their care journey. As it stands, patients frequently report feeling let down because of the variable familiarity and continuity of care, meaning they must repeatedly tell the same story.
2. What can be done to improve stroke care equitability?
Senses were heightened about inequalities during the COVID-19 pandemic, but there is a general feeling that we are starting to lose that level of enthusiasm. We discussed how vital it is to maintain and reinforce the collective feelings of frustration and sadness directed towards inequality required to tackle this challenge.
-
Using data to reduce the stroke care atlas of variation
When considering population health, technology can help turn data into intelligence by considering factors that introduce equity. For example, insight can be gathered to understand what makes an informed patient vs. uninformed patient, how access in terms of capacity and capability can be improved, geographical differences, or levels of digital immaturity.
-
Considering the pathway for patients with multiple morbidities
In many cases, stroke patients will have multiple conditions that all need managing, but multiple morbidities mean people risk being screened out of the pathway and there can be significant inequities if a patient is put onto one pathway instead of another.
An area in which technology is already seeing value is that it can help to facilitate joined-up care. Technology can help to enable multi-disciplinary teams (MDT) to work more effectively in the co-management of a patient. It is now very straightforward to host MDT conference calls rather than each consultant treating the individual conditions in isolation.
-
Establishing a consistent standard of approaches
As it stands, highly effective treatment is still unavailable to 90% of the country 24/7. For example, there is no guarantee thrombectomy will be provided to patients when needed, either due to resources or priorities. Aside from resource and cultural issues, there is a real need to define and maintain a consistent standard of approaches to reduce this variability in care provision.
3. How can we inspire change?
A big problem is that it is often not seen as a priority, therefore, it does not necessarily receive the investment it requires. Stroke is a high burden, but often receives minimal support. How do we frame the information we have to construct the right messaging and raise it as a priority issue?
-
Leverage the business case
The monetary impact of improving stroke care is clear, but sometimes overlooked. For every extra year of longevity that can be created, the UK economy will benefit £60 billion, so prevention is certainly economically viable.
-
Inspiration of a goal
History tells us that change has typically occurred from inspiration of a goal, for example, tackling hospital acquired infection motivated world leaders to change pathways. As such, there needs to be a level of frustration at the status quo balanced by unwavering focus on the end goal to achieve real change.
-
Patient stories at the heart
Bringing people back to basics and reminding them of the real reason they are there by creating common narratives about patients can not only motivate political change and social movement, but also improve workforce culture by helping clinicians find ways to say yes rather than no.
Technology is at the heart of solutions
There is a real need to look at what happens to the patient post-discharge and consider the end-to-end care pathway, including rehabilitation, in a more holistic way. Clinical staff have seen great benefits of applying technology and digital offers solutions to tackle the heart of the challenges faced within nursing and therapist communities in stroke care. Moving forward, we need to expand our applications of where particular modalities of technology-enabled healthcare have seen success; for example, telemedicine, data and understanding intelligence, visibility of resource and understanding immediate availability of workforce capacity.