Emergency services are facing huge challenges that hinder service provision; increased demand, workforce shortages, and misallocated resources are significant issues that need immediate attention. There is collective recognition that technology can play a key role in mitigating these challenges, including through:
- Avoiding admission by connecting clinicians to remote specialists to treat them on scene
- Empowering non-clinical staff to provide an on-scene response by connecting them to remote supervision and support
- Improving patient outcomes by getting multiple eyes on scene and ensuring quick treatment
However, emergency service departments have often taken a siloed approach to digital adoption, and as such have seen varying degrees of effectiveness.
To build on our previous emergency services roundtable in December 2021, we recently reconvened key senior stakeholders across the global emergency service landscape to develop our discussion around digital transformation in healthcare. Here, I have summarised my key takeaways from the discussion, including the challenges being faced, the effectiveness of current solutions and what an ideal future might look like for emergency services.
1. The huge demand on primary care is causing the public to seek help from alternative emergency services
Our previous roundtable noted unsustainable levels of demand and intense workforce fatigue. Unfortunately, this demand is showing no sign of subsiding, and as workforce fatigue is compounded by workforce shortages, it is becoming increasingly unmanageable.
As the first port of call for members of the public, primary care is suffering more pressure than most. When people struggle to contact their primary care provider, there is a multiplier effect on searching behaviours of the public. They seek alternative ways to get help and as such turn to other emergency services.
The direct impact of this can be observed in an increased number of 111 calls. Data demonstrates 111 calls now ramp up significantly earlier in the day as people seek help due to not being able to get through to primary care services. If a patient is calling 111, they have run out of all other options but need an emergency response immediately.
Emergency service leaders are asking: how can we manage this demand by deflecting patients into other pathways?
2. Using technology to connect emergency services can help to alleviate workforce shortages
Police and fire resources are already occasionally used to support the NHS by responding to health emergencies; however, leaders recognise that it can be intimidating for non-clinical staff to deal with an unwell patient on the street. Having remote specialist clinician advice would help, but consistent supervision and support amongst a distributed professional, highly autonomous, workforce is very challenging. Technology can and will support this important agenda that improves quality, safety and when handled right, support clinician wellbeing.
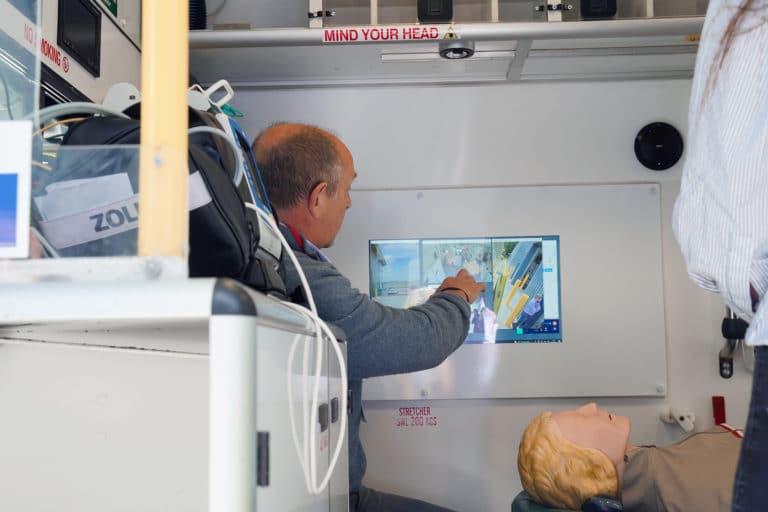
Technology can also assist by facilitating conversation at the scene, connecting on-scene paramedics to clinical advice lines and the wider medical community. As it stands, the challenges at handovers in Emergency Departments are causing backlogs in pressure and leading to further delays. Facilitating on-scene connection to remote specialists would not only help to determine the appropriate pathway and reduce unnecessary admissions, it would also empower clinicians with access to all the information they need and therefore reduce handover delays.
3. The ‘change challenge’ requires a shift in legislation and intra-agency cooperation
There is collective recognition that we can and should utilise resource from different emergency service departments to respond to calls more effectively. There is considerable capacity within firefighters and areas of other emergency services, so how can we utilise capacity effectively and where it is needed?
Implementing this change requires a redesign of services and faces political and cultural resistance. However, within the services there is a consensus that they should be shifting towards medical response. In one region, nearly 40% of calls to control are to assist in some form of medical response. This is not mandated, but evidence of a positive cultural shift.
Technology is already offering promising solutions to empower non-clinical staff to support with medical response. For example, embedding iPads with software has enabled police to respond to behavioural health calls and helped to relieve pressure on paramedics.
Although there is already evidence of deploying alternative services to support demand, to date it has been fairly unconscious and haphazard. We need to move to a clear plan which will require changing legislation and intra agency cooperation.
What would an ideal future for emergency services look like?
Although digital plays a key role in enabling solutions, it is clear that shaping the ideal future of emergency services depends largely on a cultural shift rather than technological advances. Digital solutions are developed and ready to use, however, culture and risk-aversion remain as barriers to implementation.
-
Mindset shift
Leaders must focus on cultural change to move away from the mindset of “it’s always been this way”. The technology is advanced enough for application, but services need the support of policy makers to encourage its utilisation.
There also needs to be a mindset shift in relation to resource allocation. For example, redistributing resource needs to not be about disempowering front line workers but instead about improving their skills.
-
Involving users in the design of solutions
One approach to facilitating this mindset shift is to alter how change is talked about so it is not seen as a threat or risk. If the technology is not something that is being used every single day, it will not be reached for it in that ‘one off’ occurrence. As such, it needs to be something that is routine, comfortable and familiar. Involving users in the process development will work to ensure the output is something that will be used for all/most of the follow on use cases.
-
Consideration of the entire care pathway
Visionable are pioneering a new approach to service design with their co-creation and innovation centre. Emergency service professionals are invited to use the centre to collaborate and design solutions that put the patient at the core to transform the future of healthcare delivery.
Next steps
Emergency services are already beginning to look at innovation to meet these challenges; for example, using AI to manage clinical queues, drones, and data science. However, too often services are looking at ideas in the ‘innovation space’ rather than ‘core business’. There is a need to start investing and making bold decisions to implement technology now and solve the immediate challenges. The technology is there, but there is a significant element of risk aversion – and this is where intention to change must focus.
Discover how Visionable is powering the future of connected emergency services with our Connected Emergency Services solution.