A connected healthcare ecosystem is the answer to many of the challenges faced in healthcare. An aging population, continually limited resources (both people and technology) alongside a need to use healthcare estates more effectively are just some of the reasons a digital overhaul is not just beneficial but crucial to the future of equitable healthcare for all.
What is connected health?
Imagine this. Aimee has started to experience sudden numbness in the left-hand side of her body. Her friend Becky has called 999 and an ambulance is on the way. In the meantime, Becky has been able to have a video call with the ambulance command centre, giving them eyes on the ground before the team has even arrived.
Once they do arrive, they have access not just to Aimee’s complete medical records, but also access to stroke specialist clinicians who can guide them through the best immediate care Aimee needs, as well as advise them whether she needs to go into hospital.
Once at the hospital, a rapid assessment has reduced Aimee’s door-to-needle time. Aimee’s time in hospital is reduced. Her long-term outcome has been improved because of the rapid response, and she is sent home.
Once home, her care continues, and she receives rehabilitation in the form of virtual support groups and outpatient care from brain injury specialists. Information and specialists can support and enable those clinicians providing her care easily and securely. This moves the A&E specialist from the hospital and into the community, speeding up critical care and reducing the number of patients needing hospitalisation.
What is a healthcare ecosystem?
Ecosystems reshape and disrupt industries. They are a complex of interrelationships between various parties, within a unit of space – or in this case, healthcare.
They should include all patient touchpoints in care pathways. When a citizen needs assistance with healthcare issues, in any form, the healthcare ecosystem should come into play. Eco-systems include healthcare workers, as well as the buildings and tools they use to do their job, including pharmacists, GPs, care home workers, carers, surgeons, hospitals, paramedics and their ambulances, and so on.
What is meant by ‘connected healthcare ecosystem’?
A connected healthcare ecosystem supplies healthcare workers access to data and technology they need across the care pathway to do their job effectively and efficiently, ensuring the security and validity of the data.
Connected healthcare ecosystems should be built around effective access to data, therefore data is the core backbone of any healthcare ecosystem making secure connectivity to that data the essence of such a system. Healthcare workers are time-poor needing fast, easy, and secure access to tools and information that assist them in their jobs, delivering state-of-the-art healthcare in line with patient’s needs and expectations, is the ultimate goal of a connected healthcare ecosystem.
A connected healthcare ecosystem has the potential to:
- Provide personalised and integrated care to patients
- Improve patient outcomes
- Enhance the use of critical people resources
- Reduce the stress and pressure on critical staff
- Move care into the community and out of the hospital
- Save money
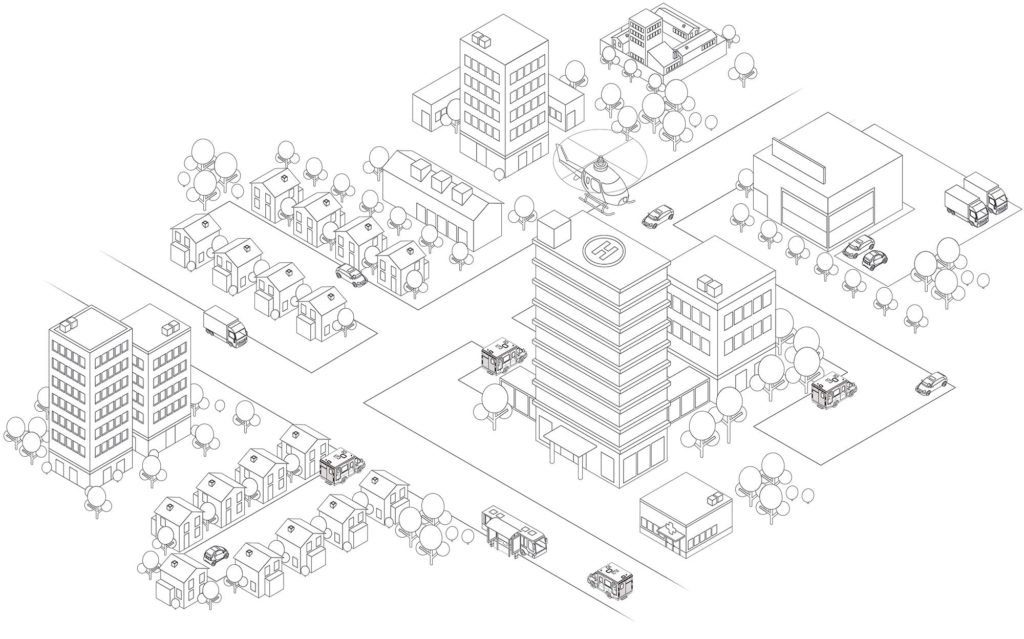

 University hospitals
University hospitals
Access to global experts for medical education and research.

 Care homes
Care homes
Direct connection to hospitals for advice avoids unnecessary admissions.
 Social care organisation
Social care organisation
Patient-centric care improved by enabling remote attendance at MDT meetings.

 Patients at home
Patients at home
Supports rapid diagnosis and prepares ambulance crew pre-arrival for immediate turnaround.
Also enables access to the right resources for bespoke recovery and rehab plans to improve patient outcomes.
 Patient visitor
Patient visitor
Virtual visiting link for family members lowers infection risks.
Also reduces transport issues for visitors and takes pressure off hospital infrastructure such as parking.

 GPs / Pharmacies
GPs / Pharmacies
GPs and healthcare professionals can connect to patients at home,
in hospitals, and even in ambulances. Gives GPs and Pharmacists access to specialist expertise.


 Hospitals
Hospitals
Rapid assessment reduces the Door-to-Needle (DTN) minimising delays in receiving appropriate treatment.
Also improves consultant liaison, community MDT support, and increases rehabilitation and outpatient capabilities.
 Shopping centres
Shopping centres
Patient convenience enhanced by virtual drop-in clinics from kiosks.

 Prisons
Prisons
Direct connection to hospitals allows appointments and
specialist advice without requiring manpower for escort duties.

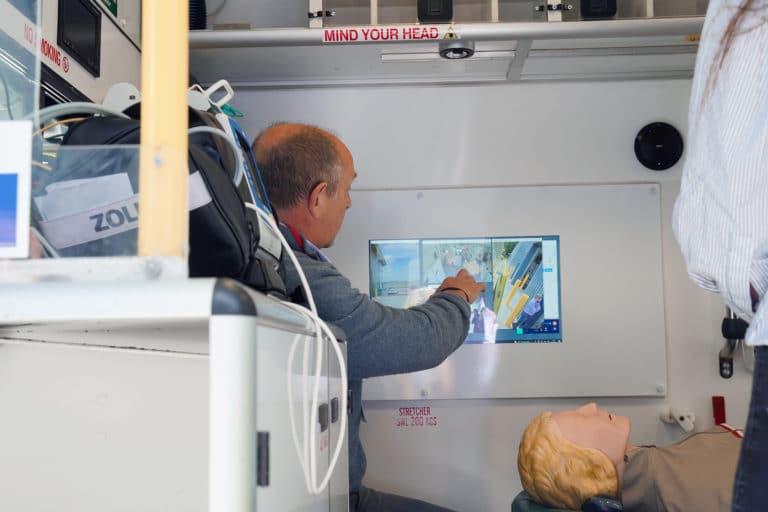
 Ambulances
Ambulances
Providing paramedics with real-time expertise in life-threatening situations.
Link with consultants supports fast positive or negative diagnosis and decision to leave home.
Air Ambulance
Provides real-time expertise and diagnostics in the most
time-sensitive and life-threatening situations.
What is an example of a connected healthcare eco-system?
The patient journey through the potential stroke pathway is a good example of a connected healthcare eco-system. But how does this look from a healthcare worker point of view?
Once Becky has called emergency services for her friend Aimee who has had a suspected stroke, the command centre can send her an invite to a video consultation. The command centre can link a specialist to the scene before paramedics have even arrived, saving precious minutes.
Once the emergency team has arrived, Aimee’s vitals can be taken and shared with the command centre and any specialist already involved in her care. Wearables on the team can help a stroke specialist decide if Aimee is in fact suffering from a stroke and decide on her conveyance, easing the pressure of not just the ambulance service, but A&E and any other services that can get clogged with patients in the wrong place.
Once a decision has been made, the paramedics can use 4G/5G or satellite to connect with specialists at the hospital they are taking Aimee to. At the same time, if that hospital doesn’t have a specialist on site, another can be contacted from another hospital. The paramedics can prepare everyone who will be involved in Aimee’s care, before they even arrive, ensuring she gets prompt and specialist care, no matter where she is taken.
Once at the hospital, Aimee is taken to a ward where a nurse sets up a telemedicine cart as there are no stroke specialists available in the hospital at that time. Although an assessment was done in the ambulance a more in-depth assessment is still needed. The nurse connects with a specialist who works with several hospitals from a central location – ensuring their specialist knowledge is exactly where it is needed to be, without needing to be there in person; these specialists can work between many hospitals in any one day. A decision is made to thrombolise Aimee. The outcome for Aimee is that she was treated in a short door-to-needle time, meaning Aimee is saved from some more long-term effects and can leave the hospital sooner, reducing cost and the strain on wider healthcare services.
Multi-disciplinary team meetings about her case are held virtually, meaning attendees can attend from anywhere and specialist knowledge can be shared much more easily. Aimee’s physio looks to seek the knowledge of a global expert in America. They attend a lecture were over 200 physiotherapists attend from all over the world and share their knowledge on the subject. This is used to improve Aimee’s rehabilitation process and other patients needing similar care.
During her stay, Aimee can safely connect with loved ones who can’t travel to the hospital through an easy-to-use virtual visiting tool and an iPad. Her mental health is much improved because of this access.
Specialist knowledge has been utilised from afar, the patient outcome has been improved, a bed has been freed sooner and money has been saved.
But a connected healthcare eco-system goes way beyond acute risk. Aimee’s journey continues at home, where she is provided a recovery program personalised to her. She has access to online peer-to-peer support groups, virtual mental health services and access to educational material, all from the comfort of her home. Information regarding her progress is shared and a program tailored to her individual needs. She also has online access to communicate with her local pharmacy, who are also connected to her GP.
If Aimee didn’t have internet access at home, her local shopping centre provides virtual drop-in clinics from a kiosk, meaning she can still access care conveniently, but isn’t required to go to hospital. Her care is connected from all angles at every stage of the care pathway, from the moment she needs care.
What is needed for an effective connected healthcare ecosystem?
Digital development is at the heart of building a connected healthcare ecosystem, but perhaps even more important than that is an enthusiasm for acceptance and success supported with systematic preparation.
A comprehensive network architecture is needed that might include:
- Secure and reliable wired or wireless access
- Cloud technology with low latencies
- Software that improves efficiency in all areas
- Data processing capabilities and analytics that include machine learning and AI (Artificial Intelligence) to supply better insight.
- Care pathway solutions that truly ease the pain points and inefficiencies for time-poor clinicians.
World class connectivity is clearly needed to meet the demands of healthcare, but so is an in-depth knowledge of clinical processes from solution providers. Upgrades to operating models and technology across layers are necessary, as well as a planned program that helps to shift behaviours of healthcare staff, to ensure connectivity is successfully embedded.
How are Verizon and Visionable working to create connected healthcare eco-system solutions?
Verizon are world class experts in connectivity and Visionable specialises in solutions designed specifically for healthcare. Together, we bring a depth of knowledge in healthcare and technology-enabled infrastructure that can revolutionise healthcare and reimagine global healthcare for all.
The partnership is designed to empower patients and make it easier for clinicians to deliver care when and when it is needed through:
- reliable connectivity that makes virtual healthcare at scale a reality.
- allowing for effective collaboration that ensures expertise is shared globally
- access to high bandwidth and incomparable imaging capabilities, ensuring efficient and personalised care
- guaranteed security with innovative cyber security and end-to-end encryption.
Collaborate and co-create in our Connected Healthcare Centre
Visionable and Verizon have built a cutting-edge co-creation and innovation centre to create an immersive experience of the connected future of healthcare.
Visitors can experience first-hand how our unique technology underpins the entire care pathway, from virtual wards to in-person care, all supported by secure and reliable 5G Verizon Connectivity.