Visionable has convened a series of roundtables to discuss the rapid roll-out of healthcare technology during the Covid-19 crisis, and what can be done to sustain progress. Former NHS CIOs and Visionable advisers Rachel Dunscombe and Andy Kinnear talk over the latest call, which discussed the challenges and opportunities ahead.
Andy Kinnear: We saw a lot of great work during Covid, but one of the things that struck me is that we saw more adoption than innovation. The NHS rolled-out remote working and virtual clinics because it had no choice; but collaboration software and video conferencing are not new. The environment had changed and forced adoption of proven technology
Rachel Dunscombe: I think that is an interesting point. We had some digital adoption before Covid, but only in some areas and in some pathways. What Covid gave us was scale and pace. The challenge now is to maintain it. To keep rolling forward and not to roll back.
‘Let’s not get into navel-gazing’
Andy: What we heard in the latest round table was concern that we could slip back. One of the GPs on the call said he was getting pushback from practices that don’t want to continue with digital-first. One of the acute CIOs said her trust is looking at waiting list recovery models built around trying to run more traditional outpatient clinics.
Rachel: I think this goes back to adoption and innovation. The GP you were just talking about said one reason that some practices are pushing back is that digital has increased their workload because they are trying to add it into traditional ways of working.
He argued these practices are trying to deal with the same patient on a consultation platform, a telephone or video call, and then face to face, when they need to triage more effectively. Which means more innovation, not less.
Andy: The challenge is that a lot of the factors that made it possible to adopt quickly last spring are making it difficult to do that now. On the call, we talked about how the flat decision-making structures that were prevalent during the pandemic are getting complicated by the reimposition of the old cumbersome governance regimes.
Rachel: We also talked about integrated care systems and how there is a danger that they could get bogged-down in debates about who sits on which board. I liked the message from an ICS CIO who said: ‘Let’s not get into navel-gazing’. We know, professionally, that moving care closer to home is the right thing to do. We need to stay focused on making that happen.
A set of levers to pull
Andy: We do need to think about board-level leadership, though. I’ve heard of ICSs not offering local IT leads board-level positions, and that’s very disappointing. During the pandemic, boards really seemed to wake up to the potential of digital and it’s vital that they don’t go back to sleep again.
The positive is that this has been recognised by the centre. NHS England says its new chief executive must drive digital. Health Education England has been working with NHS Providers on a training programme for boards. The Care Quality Commission is committed to this as part of its ‘well-led’ reviews. So, we have a set of levers pull.
Rachel: Alongside that, the professionalisation of informatics is very important. At the first round table, we talked about the professionalisation of medicine and nursing and how it would be unthinkable for a board not to have a medical director or a nursing director. We need to get to the same point for informatics, because we are the people who will make transformational care possible.
If you invest in IT, you can make savings elsewhere
Andy: Another factor is funding. One of the ICS leaders on the call said that during Covid she had been able to order iPads and pulse oximeters by the truckload. Now, the NHS has been told to revert to something close to its pre-Covid budget, and I’ve heard of IT directors being told to take ‘their share’ of their organisation’s cash releasing efficiency savings target and deliver cuts of 7-8%.
That’s bonkers for two reasons. First, because if you make an investment on the scale of the investment that we made in IT last year, you are going to have to keep spending to maintain it. Second, because if you invest in IT, you can make savings elsewhere. You don’t need so many outpatient clinics if you are monitoring people remotely. You don’t need so many booking clerks if you are booking online.
Rachel: We also talked about the need to make sure that financial incentives are aligned with new ways of working. On the call, people pointed out that commissioners will pay hundreds of pounds for an outpatient appointment, but they’re much less keen to pay for a remote monitoring follow-up. And GPs are worried about ‘losing’ capitation-funded patients to digital-first providers.
That got us into a very interesting discussion about whether the NHS should have a dedicated IT strategy and dedicated IT funding streams, or whether organisations should fund digital from their own budgets, to encourage them to adopt systems that would deliver real efficiency and clinical benefits.
Andy: Opinion was split, wasn’t it? We had one ICS CIO who thought this was the only way to get organisations to make digital part of business as usual, and we had an acute CIO who thought health tech is not mature enough to do that, yet. She suggested NHSX could look at what healthcare organisations globally spend on IT and digital teams, to encourage trusts to move in that direction.
Rachel: There’s a technology component to this, as well. One of our acute CIOs said she’d been looking at which of her hospital’s departments have gone online and which haven’t. Ophthalmology has embraced digital first; cardiology not so much.
One reason may be that systems were available in one area and not the other. On the back of that, we also talked about needing an open and transparent procurement regime that doesn’t enable one or two companies to capture whole segments of the market. We need to innovative SMEs like Visionable to bring new ideas to the table.
Andy: This whole space is moving very quickly. If you’re working in an acute trust, you can still go out and buy a mega-suite electronic patient record, but the future is open platforms that share data with an ecosystem of apps and analysis tools.
My view is that the 2020s will see an increasing move to open platforms built on open standards. So we will need a procurement regime that recognises that and doesn’t tie people into old ways of thinking.
Rachel: I’m sure we are going to get to that inflexion point and when we do it will open up a new world of opportunities. The round table was excited by automation. A mental health IT lead said his sector is already moving in this direction, by triaging patients with anxiety or sleep disorders into online support.
His mantra was that if the NHS is to cope with the demand being put on it other sectors will have to ‘let the computer do the work that doesn’t have to be done in person.’ This led us into some big-picture thinking on workforce. How is the NHS going to attract digital talent – and pay for it? What does a digitally enabled workforce look like?
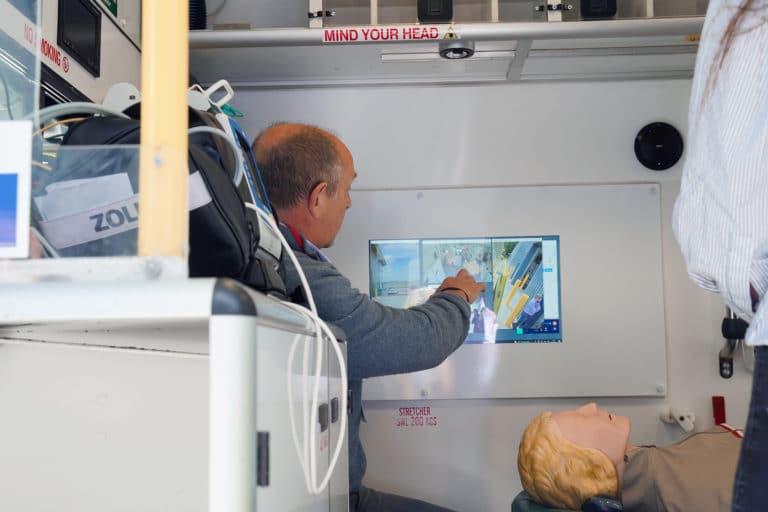
As one of our participants put it: if AI can read scans better than people, and we are going to have driverless vehicles running about, we need to work out what radiologists and ambulance crews are going to do in the future. Which means aligning the NHS digital and people strategies.
Andy: On a positive note, the NHS can be very adaptable. I led a shared care record called Connecting Care in Bristol, and when we started we had GPs saying they wouldn’t give us ‘their’ data, and after ten years we had the same GPs saying they were recording information in a different way so colleagues in other services could use it. This is the adaptive change Wachter described in action.
Rachel: We have come a long way just in the past year. I’d really like to pay tribute to all of my CIO colleagues out there for what they achieved, and I’d like to pay tribute to the UK businesses that stepped up. Some of the work that Visionable did during the pandemic was amazingly impactful for me.
Supporting end-of-life care and enabling patients to be with their loved ones and faith leaders at the end of their lives was inspirational. We really saw the best of CIOs and companies, working in collaboration. We just need to make sure we can see more of the same.