Quality healthcare for prisoners and in prisons presents a myriad of challenges. But which pain points could be solved today through the use of technology?
In this blog, we explore the problems clinicians, prison staff and prisoners commonly experience and how those problems can be solved using technology already being used by HMPPS.
5 issues in prison healthcare and how to solve them
Ensuring the population of nearly 80,000 prisoners* in the UK is provided with the same healthcare and treatment as anyone outside of prison, as required by law, is a challenge for prison staff and the NHS alike. The following are some the biggest challenges facing prisons today as well as how technology could be used to support a new approach.
1. Providing the same level of quality and access to care
Her Majesty’s Prison and Probation Service asks that a “minimum standard escort strength” for prisoners visiting a hospital or healthcare establishment be “two officers or more, with restraints applied to the prisoner in all but exceptional circumstances.”
With this standard in place for the safety of everyone involved, the capacity to escort prisoners to healthcare appointments as and when they need them becomes extremely limited. There just are not the necessary numbers of staff free to tend to one single prisoner.
The Nuffield Trust research into prisoner healthcare found that,
“Prisoners use hospital services far less and miss more hospital appointments than the general population… Prisoners had 24% fewer inpatient admissions and outpatient attendances than the equivalent age and sex demographic in the wider population…”
They also state, “a significant part of this gap may be explained by prisoners having poorer access to services, with the limited supply and availability of escorts… being a key factor.”
Public Health England (2019) also found the same issue in their study of prisoner’s access to dental services.
Using technology to reduce the number of escorts needed for prisoner healthcare appointments
They say, ‘Necessity is the mother of invention’, and the COVID19 pandemic was that for the prison service and the need for quality accessible telehealth services. HMPPS invested in and continue to use Visionable as a means to connect NHS clinicians, prisoners, and prison healthcare teams to improve prisoners’ access to healthcare. There is no need for escorts, and specialists can be located anywhere, meaning better quality of care and much greater accessibility for patients.
2. Encouraging engagement and continuity of care
In Public Health England’s Guidance for improving continuity of care between prison and the community, it is stated,
“An integrated care pathway from prison to the community is crucial for supporting recovery from substance misuse and reducing reoffending among people leaving custody.”
Despite this, the same guidance states, “Current PHOF indicator 2.16 and section 7A data provides evidence that successful transfer of offenders to substance misuse treatment in the community is low (30%).” The guidance provides a number of reasons for this low rate including,
“Almost half of the referrals made by prison treatment services were not received by the community treatment services,” and “limited opportunity to make referrals with unplanned releases from court and no joined-up working with probation services during release planning.”
Using technology to encourage engagement and continuity of care
Clearly there is a need for a more joined-up approach to healthcare in prisons and beyond to ensure patients are encouraged to continue their care beyond the prison walls. All of HMPPS in England have already implemented Visionable, and as we already work with the NHS, it is easily incorporated into existing IT systems there too.
The use of telehealth also means that the transferal of a prisoner from one end of the country to the other doesn’t need to mean disruption of care. Prisoners can remain with their local healthcare provider, no matter which prison they are in, or where their healthcare provider is.
3. The negative experiences of healthcare for prisoners
“It is kind of like parting the red sea when you walk into […] the hospital with handcuffs on. Everybody gets out of your way, parents grabbing their kid out of the way and things like that because, I can understand that just seeing handcuffs is not a good look at all.”
“Sometimes people do complain that we’re sitting there, and they might make comments.”
“And they struggled to find a place for me to wait and what happened is they found like a broom cupboard where I had to wait which was definitely degrading. I’m valued less than a normal person.”
These three separate accounts are from prisoners describing their experiences visiting hospitals. They feature in the below video from the UCL Institute of Epidemiology and Health Care.
Patients that attend hospitals from prisoners are faced with the stigma of appearing in front of the greater population wearing handcuffs, which are often only for the prevention of escape rather than potential danger. A more dignified approach could help prisoners engage more fully with the healthcare systems.
On top of this, appointments are often attended by officers as well as the prisoner, meaning there is a severe lack of privacy. For female prisoners in particular, it is common for one of the officers present to be male, which can be both intimidating and humiliating.
Using technology to provide a more dignified approach to care
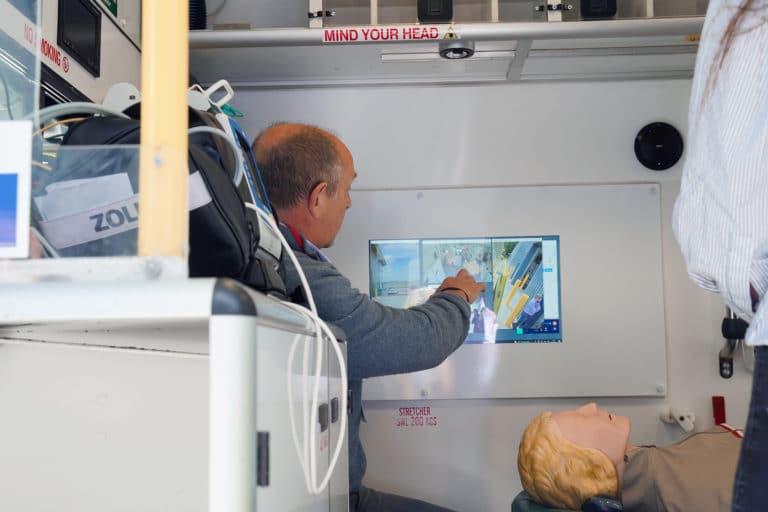
Using Visionable, HMPPS provide patients with a prison-based healthcare worker and connect them with a clinician remotely. Telehealth allows the prisoner the dignity to attend a healthcare appointment away from the greater population, as well as giving them the privacy they need by negating the need for officer chaperones.
4. The cost to provide healthcare for prisoners
Because each trip to a hospital requires two escorts at a bare minimum, and sometimes a member of the prison healthcare team, the cost can be huge. The prison staff who act as escorts must travel, wait at the hospital, travel back, and do the same again with the next prisoner. This is a huge weight to bear in both cost and resource. Compounding this further, long travel is sometimes required as prisoner transfer across the country is common.
Using technology to reduce the cost of prison healthcare
Telehealth helps to significantly reduce the cost of transporting and escorting prisoners to healthcare services. In addition to this, because HMPPS is already using Visionable, there is no added cost for hospitals to use the software system.
5. Risk of security beyond the prison walls
Escorts and handcuffs are used to ensure maximum security is maintained whilst prisoners are attending appointments beyond the prison walls. However, it is impossible to maintain the same level of safety provided by a prison once a prisoner has left the building.
Using technology to increase security and safety
Using telehealth services removes the security risk as prisoners can remain on prison property, within their own cell, to receive most healthcare treatments.
However, it is incredibly important for telehealth services used with HMPPS to be digitally safe and secure, which is why many prisons use Visionable. Visionable does not store any personal identifiable data and is end-to-end encrypted, protecting both clinicians using the platform and patients’ healthcare details.