Dr Zoe interviews Dr Deborah Cunningham, who has been a consultant Radiologist for over 40 years, to find out more on her experiences of working from home using Visionable technology to participate in breast cancer multidisciplinary team (MDT) meetings. All this whilst self-isolating at home (Dr Zoe also discovered how Deborah managed to get BT to install emergency fibre broadband in her house in a matter of days).
Across the NHS, clinicians have been experimenting with new ways of working during the Covid 19 pandemic. For me, as a GP, the majority of consultations have been over telephone or video call. I’ve been chatting with GP colleagues and unanimously we agree that it is highly unlikely that we will go back to our old way of working. Whilst the in–person, face-to-face consultation remains the gold standard in many circumstances, it has become clearly apparent that this is not the case for a significant proportion of the GP daily workload.
Both GPs and patients have been finding a new level of willingness and respect for the virtual consultations, especially so amongst younger patients who have straightforward presenting queries or complaints. Is it becoming normal practice for GPs to work some of their sessions from home, with a laptop. Whilst I can see and make sense of a more digital world in future primary care, my brain boggles when it comes to making sense of how hospital medicine can be carried out from home.
Doctor in the house
I got the opportunity to catch up with Dr Deborah Cunningham, a consultant radiologist (x-ray Dr) for over 40 years, who specialises in breast cancer diagnosis, treatment and research at St Mary’s Hospital, London. Until recent times a typical day’s work for Deborah, like most doctors, was in a clinical setting. But since the government advised certain groups to stay at home to protect themselves, her and her husband have been self-isolating together at their home in Hertfordshire.
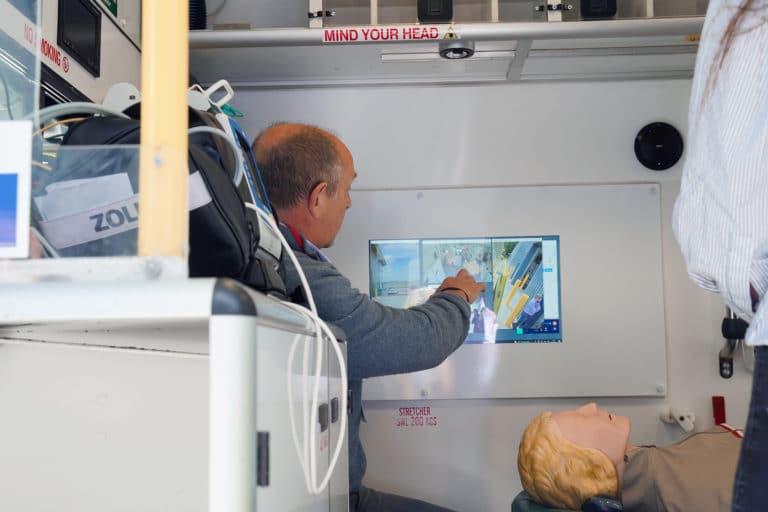
You’d be forgiven for assuming that this situation would render Deborah, as a Radiologist, ‘unable to work’, but in actual fact she has continued to work, despite self-isolation, by using Visionable technology. Deborah has been able to review x–rays from her own home, which has freed up her hospital-based colleagues to come out of their reporting rooms and work on the Covid wards, where their contribution was so desperately needed. In addition to this, and of high importance to Deborah, she has still been able to contribute and be present (virtually) at breast cancer multidisciplinary-team meetings, where her super specialist knowledge and skills are of the utmost value.
Deborah’s informed me that the MDT meetings typically last for 3 hours, will be attended by 25 clinicians, including not just one, but several surgeons, specialist nurses, oncologists, pathologists and radiologists, with between 50-100 patient’s cases being discussed in each meeting.
Deborah’s expertise as a radiologist who has sub-specialised in breast cancer care, make her irreplaceable at these particular meetings. I asked Deborah how difficult she had found the introduction of this new technology and this new way of working, she said:
“I think it is quite easy… There are lots of other group meeting options out there, but Visionable, when used for the multidisciplinary team meetings, is incredibly secure. And with few technological problems, it is really easy to use and decide what you’re going to show to other members of the group, and see what others are looking at.”
No longer the technophobe
In a previous blog I spoke about how I am a technophobe, Deborah is clearly savvier than me, but she is by no means a technology enthusiast either. Until very recently her and her husband got by with minimal broadband bandwidth at home – an unfathomable state of affairs for the typical technology guru. Hats off to her husband though, who used his powers of persuasion and communication of the importance of Deborah’s role to BT, who arranged for fast fibre to be fitted within a matter of days. And rightly so.
Although by her own admission turning to technology was out of necessity, rather than choice, she appreciates the power and importance of having systems in place like Visionable. As a doctor, she admits that her preference would always be to work inside the hospital so that she can communicate with her patients and colleagues in person, but realises there are times when these ‘new ways of working’ are a god send, and are effective, simple, and secure.
She gave me one example:
“When it comes to reporting on x-rays the images are instantly available and the picture quality is perfect, and I am able to use the same voice recognition system for reporting as I would normally.”
So, there we go, hospital medicine from home!
In these unprecedented times, the NHS has embraced technology and the working from home culture, like never before, in both primary and secondary care. It does seem evident that things may never be the same again, and dare we say, that some of us (clinicians and patients), possibly even prefer it. But in Deborah’s case, especially when it comes to her MDTs, she’s undeniably looking forward to getting back to the hospital.
What is the multidisciplinary team
People with breast cancer are cared for by a team of healthcare professionals, each with their own expertise. This is known as the multidisciplinary team (MDT). They will meet regularly to discuss your care at the multidisciplinary team meeting.
The team may include:
- breast care nurse – a nurse who provides information and support to people diagnosed with breast cancer
- chemotherapy nurse – trained to give chemotherapy drugs
- clinical oncologist – a doctor who specialises in treating cancer with radiotherapy alone or radiotherapy and cancer drugs
- medical oncologist – a doctor who specialises in cancer drugs
- pathologist – a doctor who examines the tissue and cells removed during a biopsy or surgery
- radiologist – a doctor who specialises in the use of x-rays, ultrasound and scans to diagnose and treat disease
- research nurse – who can discuss the option of taking part in clinical trials
- surgeon
- therapeutic radiographer – trained to give radiotherapy